Tips for Surviving the Summer of COVID with a Brain Injury
Guest post by Dr. Jaycie Loewen, PhD, MSCI, HETSC, with Cognitive FX
The COVID-19 pandemic and quarantine have created challenges for people across the world. This is, perhaps, especially true for traumatic brain injury (TBI) survivors and their caregivers who are already dealing with the physical, mental, and emotional consequences of brain injury (Wilson et al., 2017). While some TBI survivors may initially find following COVID-19 restrictions not too different from their daily lives, effects on psychological health, relationships with family and friends, and lifestyle patterns can have noticeable and long-term consequences (Jimenez-Pavon et al., 2020). In this article, we are going to address some of the biggest issues COVID-19 and the quarantine may be causing TBI survivors (especially during the summer season) and give tips on how to manage those issues.
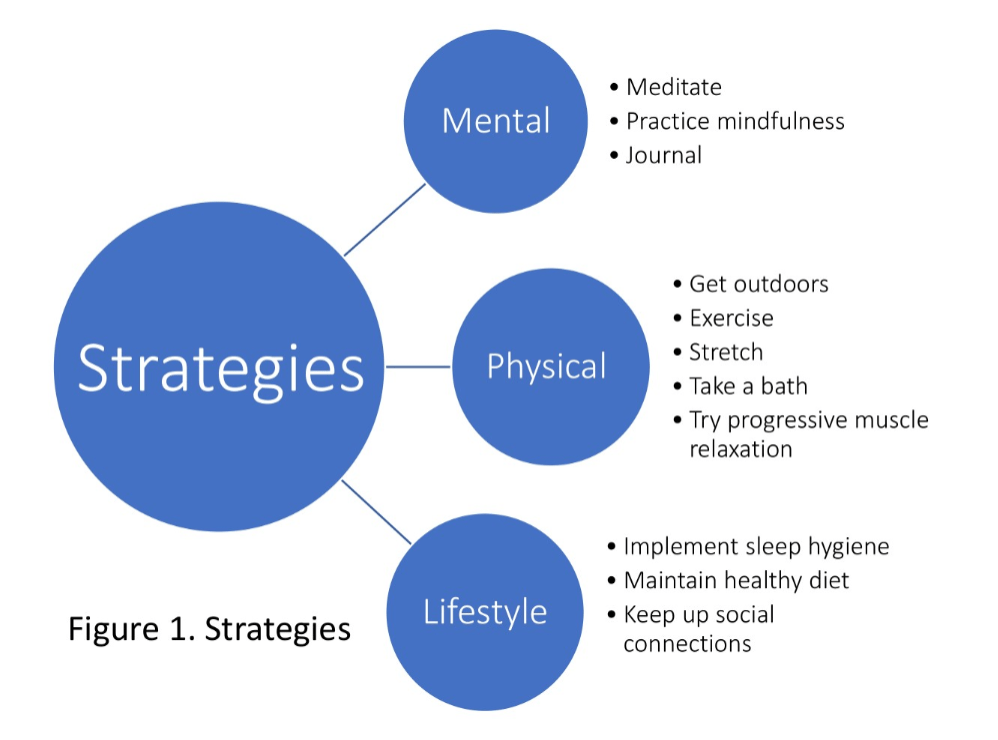
COVID-19 has already had published effects on physical, mental, and emotional health (Holmes et al., 2020; Qiu et al., 2020). These effects not only come from the threat of the viral infection, but also from changes to how we live our lives. For TBI survivors and their caregivers, these changes in lifestyle—such as being on the computer more for work, homeschooling the kids, or experiencing restricted access to social support or medical providers—will affect the ability to manage TBI-related symptoms. It may be more difficult to stick with healthy coping methods for stress and continue fostering personal relationships. In addition, quarantine can lead to less physical activity and time outdoors, causing an increase in feelings of isolation and depression. Importantly, the effects COVID-19 will have on physical and mental health may last longer than the epidemic itself (Holmes et al., 2020). The summer of 2020 will present many unique challenges; however, there are several strategies you can learn, implement, and maintain to support symptom management and overall health (See Figure 1 Strategies).
The problem: The kids are at home more
COVID-19 has caused the closure of summer schools and kid’s activity resources, which means family members are at home together more hours in the day. And even when facilities open, social distancing measures may drastically change how often you utilize the resources. On one hand, the extra family time can be great. For TBI survivors, however, this often means more noise and chaos during what normally would have been quiet, solitary hours to rest.
Solution: It is OK to take a time-out
We have heard from many TBI patients that the increased number of people and activities in the home has intensified their symptoms because of overstimulation. Our advice to these patients has been that it is all right to take extra breaks when needed. The same goes for you. Look for opportunities throughout your day to take little breaks. Perhaps you have 10 minutes while the kids are napping or watching a movie. Maybe you have just 15 minutes between Zoom meetings for work. Maybe your break can come while your dinner is cooling. Use that time to de-stimulate. Find a quiet and/or dark room if you can. Practice some slow, deep breathing. Help your mind and body slow down. Don’t be discouraged if you feel you need extra breaks to get through your day. Everyone is under extra pressure in these strange times. Be compassionate with yourself and your needs.
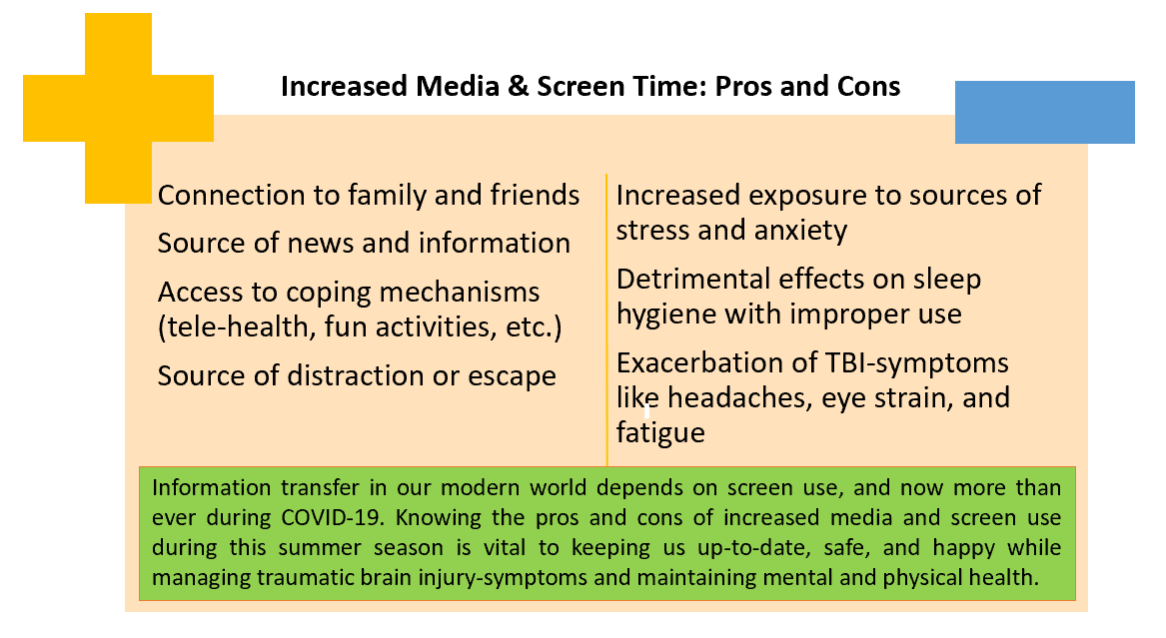
The problem: Increased screen time
Since quarantine began, screen time has increased drastically. Now, not only are people using screens for recreational activities and media, but many find themselves attending classes or working, all via digital means. Increased use can be especially problematic for TBI survivors who deal with screen sensitivity. More screen time can lead to headaches, eye pain, eye strain, dizziness, and difficulty sleeping, among other post-brain-injury symptoms.
Solution: Take a break from the screen and find new outlets
It’s healthy to follow the 20-20-20 rule (for every 20 minutes using a screen, spend 20 seconds looking at something 20 feet away). Additionally, you can break the endless screen cycle by taking a break from it when you need to. Find other healthy coping methods (see Figure 1. Strategies) for your stress. If you find yourself naturally drawn to screens for distraction, make a note to try one of these instead:
- Call a friend you haven’t talked to in a while
- Take a treat to a neighbor
- Do a puzzle or play a board game
- Cook a meal
- Listen to an audiobook
- Send your family a care package
The problem: Poor sleep
Changes in sleeping patterns has also been a problem with quarantine. More exposure to blue light sources (like screens!), decreased physical activity, and a loss of daily routines are all contributing factors. The warmer weather during summer and longer daylight hours can also affect sleep quality.
Solution: Keep up a daily routine and practice good sleep hygiene
While it doesn’t have to be as rigorous it used to be, keep your daily schedule. Be as productive during your normal active hours as possible, even if those hours aren’t spent working. Limit screen time an hour before bedtime and use blue light filters. Keep your bedroom cool (low-to- mid 60 degrees F). Limit the number of naps you take during the day, and try not to nap after 3:00 p.m.
In summary, COVID-19 has caused an obvious shift in the way the world works, and, as a result, has introduced challenges to the way in which survivors of TBI and their caregivers live. For those who find COVID-19 is affecting them currently, or for those who want to mitigate effects down the road, there are a number of strategies you can implement, no matter the season. From putting down your phone for a few hours to finally meeting that couple across the road (from a six-foot distance, mind you), every little thing helps. As this is the first summer in which our society will be adapting to COVID-19 restrictions, knowing possible challenges and their respective solutions will be key for TBI survivors who want to maintain their mental and physical wellbeing.
— REFERENCES —
Wilson L; Stewart W; Dams-O’Connor K; et al. The chronic and evolving neurological consequences of traumatic brain injury. Lancet Neurol. 2017;16(10):813-825.
Jiménez-Pavón D; Carbonell-Baeza A; Lavie CJ. Physical exercise as therapy to fight against the mental and physical consequences of COVID-19 quarantine: Special focus in older people [published online ahead of print, 2020 Mar 24]. Prog Cardiovasc Dis. 2020; S0033-0620(20)30063-3.
Holmes EA; O’Connor RC; Perry VH; et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7(6):547-560.
Qiu J; Shen B; Zhao M; Wang Z; Xie B; Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations [published correction appears in Gen Psychiatry. 2020 Apr 27;33(2):e100213corr1]. Gen Psychiatry. 2020;33(2):e100213. Published 2020 Mar 6.
ABOUT BRAIN INJURY ALLIANCE OF ARIZONA
The Brain Injury Alliance of Arizona (BIAAZ) is the only statewide nonprofit organization dedicated to improving the lives of adults and children with all types of brain injuries through prevention, advocacy, awareness, and education. BIAAZ also houses the Arizona Brain Health Resource Center, a collection of educational information and neuro-specific resources for brain injury survivors, caregivers, family members, and professionals.
What began in 1983 as a grassroots effort has grown into a strong statewide presence, providing valuable life-long resources and community support for individuals with all types of brain trauma at no charge.
The Brain Injury Alliance of Arizona:
- Works with the Congressional Brain Injury Task Force
- Houses Arizona Brain Health Resource Center
- Hosts the Statewide Opioid Use Disorder & Cognitive Impairment Workgroup
- Deploys a Statewide Opioid Use Disorder & Cognitive Impairment Response Team with peer support, training and family wraparound services
- Facilitates the Brain Health Advisory Council
- Manages a Statewide Neuro Info-Line 888-500-9165